Table of Contents
ToggleBeyond CRISPR Hype
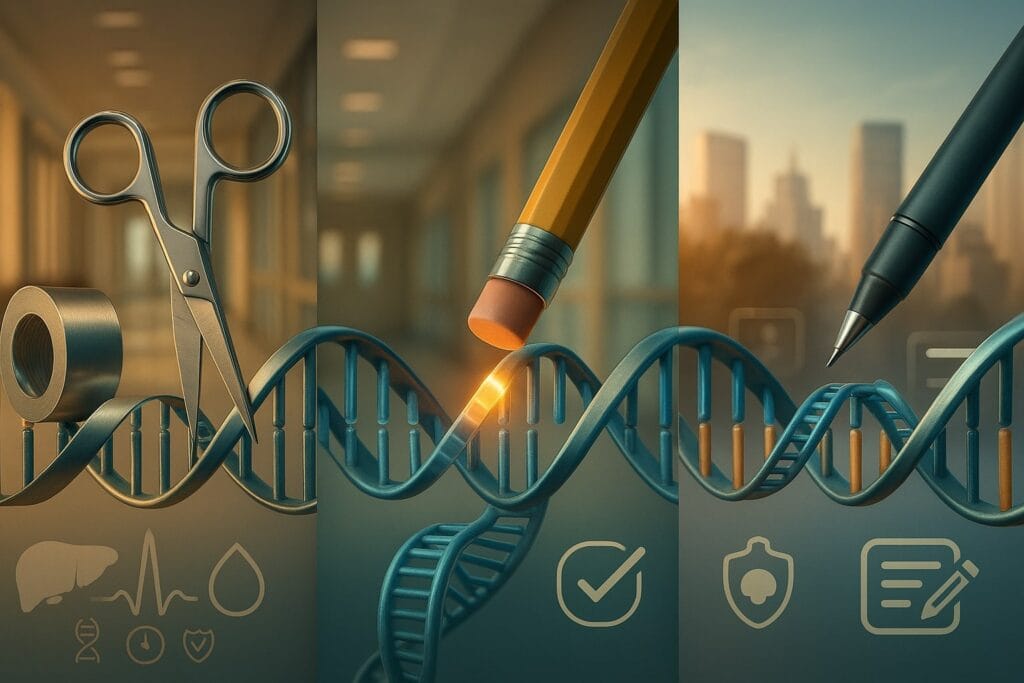
Gene editing has promised to revolutionize medicine, but only now are the next-generation tools base editing and prime editing moving from petri dishes to patients. CRISPR’s first wave – classic CRISPR-Cas9 nucleases – yielded headline-grabbing cures (like sickle cell and beta-thalassemia therapies approved in 2023). Yet those approaches make double-strand DNA breaks, raising safety and delivery challenges. Base and prime editors offer a gentler fix: they rewrite DNA one letter at a time or perform small insertions, without blunt cuts. After years of hype, these precision editors are entering clinical trials en masse. The big question: which of these experimental cures will actually reach patients by, say, 2026–2030?
“Scissors and tape” vs “pencil eraser” vs “word-processor rewrite.”
—Dr. Seyed Hassan Fakher, MD
“Base editing is a direct, irreversible switch of one DNA letter (A, T, C, or G) to another—without cutting both DNA strands,” said Dr. Seyed Hassan Fakher, MD, in comments to Industry Examiner. “Prime editing lets us substitute, add, or delete small bits of DNA—again without a double-strand break. If classic CRISPR is scissors and tape, base editing is a pencil eraser, and prime editing is a word-processor rewrite.”
Clinical Trials Underway
As of mid-2025, at least 19 clinical trials are already testing base or prime-edited therapies. Early results are encouraging – seven trials have reported data so far, “all showing patient benefit” from a base or prime edit. The first beneficiaries have been patients with dire conditions that traditional gene therapy struggled to fix:
- Blood Disorders: Beam Therapeutics’ BEAM-101 is a base-editing therapy aiming to induce fetal hemoglobin for sickle cell disease (SCD). In its Phase 1/2 BEACON trial, over 40 patients have been treated, with robust engraftment and rising fetal hemoglobin levels reported. They expect to dose 30 patients by mid-2025 – a milestone that could set up a BLA filing (approval request) soon after. If all goes well, Beam’s SCD cure could reach the market by ~2026–27, positioning it alongside or even competing with the first-gen CRISPR SCD therapy (Cas9-based) that received approval in late 2023. For patients, base editing might offer similar curative outcomes with potentially fewer off-target effects or complications, since it doesn’t make DNA breaks.
- Cholesterol & Heart Disease: Verve Therapeutics is deploying base editing in vivo to permanently lower LDL cholesterol. Its therapy VERVE-102 targets the PCSK9 gene in liver. Early human data in 2025 showed that a one-time infusion led to significant “dose-dependent” LDL reductions after 28 days. At the highest dose tested, LDL (“bad” cholesterol) levels plunged – proof that base editing can rewrite a gene inside the body to deliver a therapeutic effect. With FDA fast-track designation in hand, Verve aims to advance into larger trials by 2026. If the safety profile holds (no serious off-target mutations in liver or elsewhere), a cardiology-focused gene editor could reach patients by 2028–2030, offering lifetime cholesterol control and possibly preventing heart attacks in high-risk individuals. “PCSK9 tags LDL receptors for breakdown,” Dr. Fakher noted. “Silencing PCSK9 raises LDL receptors so the body clears more LDL. Early candidates are very-high-risk patients who don’t reach targets or can’t tolerate statins, including familial hypercholesterolemia. So far we mostly see transient liver-enzyme bumps or immune reactions to delivery; these have tended to resolve without lasting injury in early studies.”
- Rare Metabolic Disorders: In late 2024, a medical first occurred – a baby with a deadly inherited urea cycle disorder (OTC deficiency) was treated with a personalized base editor, correcting a single DNA letter in his liver. Within weeks, the infant’s ammonia levels normalized and he was able to tolerate protein, a near-miraculous recovery. While that was a bespoke, one-off treatment (essentially a compassionate-use case), it proved the principle that base editing can cure inborn metabolic errors inside a patient. Looking ahead, Beam Therapeutics is developing BEAM-301 for Glycogen Storage Disease Type 1a, another metabolic disorder caused by a single mutation. The first patient was dosed in early 2025. If base editing restores proper enzyme function in the liver for GSD1a patients, Beam could seek approval by the late-2020s, offering the first real treatment for this currently unmanaged disease.
- Immune Deficiencies: Prime Editing – the more versatile cousin that can add or delete DNA bits – saw its first human trial in 2025. Prime Medicine treated an 18-year-old with a chronic granulomatous disease (CGD, an immune disorder) by inserting two missing DNA letters in his stem cells. The result: his white blood cells regained 90% of normal function, effectively curing the immune deficiency. This landmark case (the first-ever prime edited patient) suggests prime editing works in human cells. Prime Medicine’s Phase 1 trial for CGD (targeting the NCF1 gene) delivered such promising early results that the edited cells produced enough protein to be potentially “curative,” with no serious adverse events. They anticipate moving to a pivotal trial by 2026 and, if partnered or funded, could achieve approval around 2028 for this rare disease. Beyond CGD, Prime is preparing a program for Wilson’s disease (a liver disorder) aiming for first-in-human by 2026, and is researching prime editing approaches for cystic fibrosis mutations– though a clinical product for CF likely lies beyond 2030 given the complex delivery to lungs. “In CGD, prime editing corrected the causal mutation, letting cells make the previously missing protein and restoring immune function,” Dr. Fakher said. “That matters because point mutations and small indels account for a large share of rare-disease variants—prime editing can, in principle, address most of them.”
Cancer and Cell Therapy
Base editing made headlines in late 2022 when British doctors used it to create “universal” donor T-cells that cured a young girl’s aggressive leukemia after standard therapies failed. They performed three precise base edits to engineer donor T cells to attack cancer while evading rejection; the patient, Alyssa, went into remission and remains cancer-free over three years later. This success is now spurring trials of base-edited CAR-T cells for refractory leukemia and lymphoma. By 2026, we may see off-the-shelf cancer therapies using base-edited immune cells reaching late-stage trials. If efficacy holds, the first approvals for a base-edited cell therapy in cancer could arrive by 2028, offering readily available cell therapy without the manufacturing wait times of today’s bespoke CAR-Ts.
Safer, Faster, Better?
What makes base and prime editing so appealing is their potential for safer and more precise corrections. Traditional CRISPR often relies on creating a DNA break and letting the cell repair it, which can introduce errors or trigger p53-mediated cell death. Base/prime editors avoid those double-strand breaks, drastically reducing chromosomal rearrangements or other byproducts. As a result, regulators have been cautiously optimistic. The U.S. FDA has already allowed multiple trials to proceed, including in vivo base editing (e.g. Verve’s therapy) and ex vivo prime editing. Still, safety will be watched closely as larger patient numbers get treated. Notably, one NIH-led trial of a base-edited cell therapy for X-linked CGD was paused in 2025 after a patient experienced a severe adverse event, prompting investigation. Such incidents underscore that even without DNA cuts, gene editing isn’t risk-free – delivery vehicles (like lipid nanoparticles or viruses) and biological variables can cause immune or insertional side effects.
Dr. Fakher framed the key risks in plain English:
- Wrong spot? Rare off-target edits at similar DNA sequences.
- Boosting efficiency? Some systems briefly dampen mismatch-repair—useful, but a theoretical cancer risk if mismanaged.
- Getting it there (then gone)? Delivery can trigger immune responses; lingering editors can raise off-target risk.
2026–2030: Milestones on the Horizon
Barring unforeseen setbacks, several base/prime editing therapies are on track to reach patients:
- First FDA Approvals: By 2026 or 2027, Beam Therapeutics could file for approval of its base-edited sickle cell cure if Phase 2 data remain strong. This would mark the first regulatory approval of a base editing medicine, likely in the U.S. or EU, cementing base editing as a mainstream therapy. Similarly, Prime Medicine’s CGD program could see approval by 2028–29, given the disease severity and lack of alternatives. These timelines assume pivotal trials show clear benefit and manageable risks. “A pivotal trial is the decisive study meant to support approval—run after early trials show promise,” Dr. Fakher said.
- Expansion to Common Diseases: Late this decade, base editing might expand from rare disorders into more common conditions. Verve’s cholesterol trial results by ~2026 will indicate if a one-shot gene edit can replace daily statin pills. Should it succeed, by 2029–2030 we could witness the first gene editing therapy for a widespread chronic illness (cardiovascular disease) entering the market – a paradigm shift from treating thousands of patients to potentially millions. Another area is viral diseases: researchers are testing base editors delivered via mRNA to knock out viral genes (e.g. in hepatitis B or HPV infections). A functional cure for HBV using base editing could be a late-2020s development.
- Personalized One-Off Therapies: An audacious vision for 2030 is routine “N-of-1” gene editing treatments for ultra-rare mutations. Pioneers like Dr. David Liu foresee a framework enabling 1000 patients with unique genetic diseases to be treated by 2030 with personalized editors. The baby treated in 2024 was proof-of-concept. To scale this, manufacturing and regulatory processes will need streamlining – perhaps with specialized pathways for individualized medicines. If achieved, by 2030 a child born with a fatal genetic error might routinely receive a custom base editor therapy within months of diagnosis, effectively rewriting their DNA and fate.
From Hype to Healthcare
In the early 2020s, base and prime editing were hailed in lab studies but unproven in humans. Now, concrete timelines are emerging. The next five years (2025–2030) should see these technologies graduate from trials to clinics for select diseases. We expect initial approvals in inherited blood and liver disorders by 2027, followed by broader indications like heart disease and possibly cancer by decade’s end. Each success will build confidence – and each setback (if any unexpected off-target effects or immune reactions occur) will guide safety refinements. By 2030, the once-hyped “single-letter DNA fixes” will likely be an established part of the medical toolkit, with patients regularly receiving base/prime-edited cells or injections. The era of genomic medicine will have truly arrived when we can ask a doctor not “can we treat this genetic condition?” but rather “which gene editor will we use to fix it?”