Early data from a tiny trial suggest that a single CRISPR infusion can cut “bad” cholesterol and triglycerides in half. The hard questions now are less about biology and more about economics, safety and who should be offered an irreversible edit in the first place.
Table of Contents
ToggleHeart disease meets “one-and-done” medicine
Cardiovascular disease remains the world’s leading killer. The World Health Organization estimates that about 19.8 million people died from cardiovascular causes in 2022—roughly 32% of all deaths globally, with most of them due to heart attacks and strokes.
Cholesterol and other blood fats sit at the centre of this story. Analyses suggest that roughly one in five adults worldwide has high LDL cholesterol, around one in four has high triglycerides, and more than half have some form of dyslipidaemia.
We already have cheap, effective drugs. High-intensity statins, often combined with ezetimibe or newer injectables, can drive LDL to very low levels and cut the risk of heart attack and stroke in half or more over time. The problem is less pharmacology than human behaviour: across multiple studies, 25–50% of patients stop their statin within the first year, and long-term persistence at five years can fall to roughly one in four.
Into this familiar landscape comes CTX310, an experimental gene-editing therapy from CRISPR Therapeutics. Instead of asking patients to swallow a pill every day or come in for injections every few months, CTX310 offers a startlingly simple proposition: a single two-hour infusion designed to permanently switch off a cholesterol-related gene in the liver.
In early November 2025, researchers unveiled the first-in-human data at the American Heart Association’s Scientific Sessions in New Orleans and simultaneously in The New England Journal of Medicine.
The headline number was easy to grasp: at the highest dose tested, LDL cholesterol and triglycerides both fell by around 50%—and stayed that way for at least 60 days—after a single infusion.
The harder part is working out what that actually means.
Inside the 15-person experiment
The phase 1 trial was intentionally small: just 15 adults aged 31 to 68 with difficult-to-treat lipid disorders—high LDL, high triglycerides or both—despite being on what their doctors considered maximally tolerated therapy. Many were already taking statins, ezetimibe or PCSK9 inhibitors.
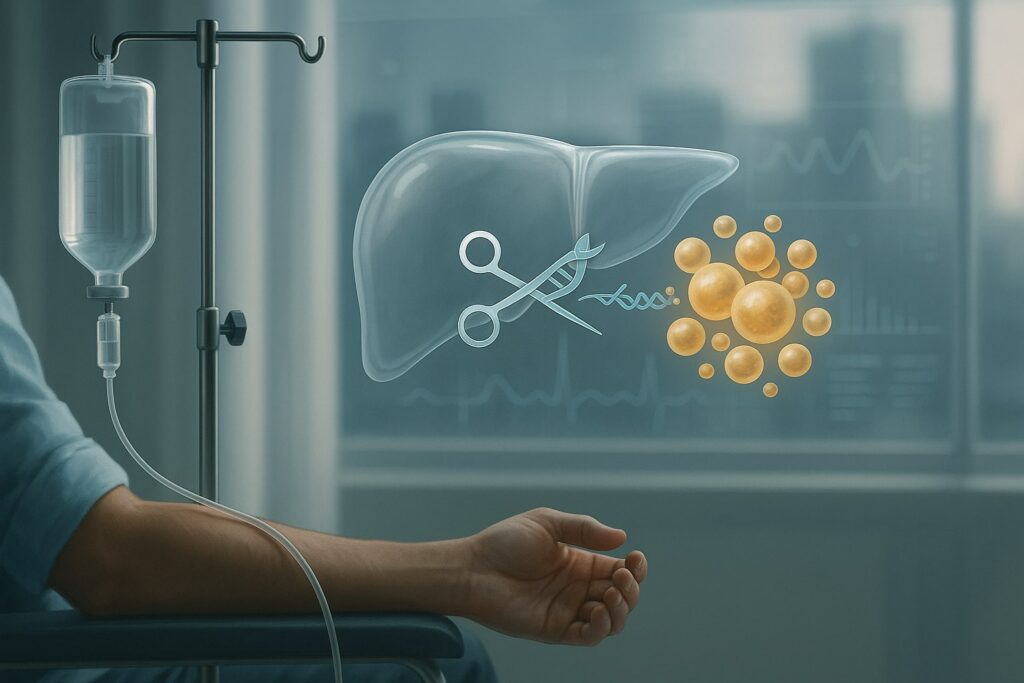
Each participant received a one-time intravenous dose of CTX310, ranging from 0.1 to 0.8 mg/kg. The drug is a lipid nanoparticle (LNP) formulation carrying messenger RNA for the CRISPR-Cas9 editing enzyme and a guide RNA that homes in on a single liver gene called ANGPTL3.
The design was classic early-phase medicine:
- Primary aim: safety and tolerability.
- Secondary aims: how much ANGPTL3 protein fell and how LDL, triglycerides and other lipids responded.
The numbers at the highest dose (0.8 mg/kg) are striking:
- Mean ANGPTL3 protein levels dropped 73% from baseline, with some patients seeing up to 89% reductions by day 30.
- By day 60, mean triglycerides were down 55% (up to 84% in some individuals), and LDL cholesterol had fallen 49% (with individual reductions up to 87%).
These changes appeared rapidly—within about two weeks—and remained stable through at least two months, the current limit of reported follow-up.
On safety, the early picture is reassuring but necessarily incomplete:
- No treatment-related serious adverse events were reported.
- There were a handful of infusion reactions (graded as moderate), one allergic reaction, and one case of elevated liver enzymes in a patient whose levels were already raised at baseline; all resolved with standard care.
- No grade 3 or higher transaminase elevations, and no CTX310-related dose-limiting toxicities.
For a first-in-human study, these are unusually clean biomarker and safety signals. But they are still, in absolute terms, just 15 people followed for weeks, not years.
Why edit ANGPTL3 at all?
ANGPTL3 (angiopoietin-like protein 3) is one of nature’s own cholesterol switches. It modulates enzymes that break down triglyceride-rich lipoproteins and influences LDL levels. People born with loss-of-function variants in ANGPTL3 typically have very low triglycerides and LDL and a markedly reduced lifetime risk of coronary disease—with no obvious adverse consequences so far.
From a drug-developer’s perspective, that makes ANGPTL3 “high-value real estate”:
- It is upstream of two major risk factors—LDL and triglycerides.
- Lifelong reduction appears both safe and protective.
- Lifestyle modification does relatively little to ANGPTL3 levels, which strengthens the case for a genetic or pharmacologic approach.
The industry has already tested this idea in a more conventional way. Regeneron’s monoclonal antibody evinacumab (Evkeeza) targets ANGPTL3 and is now approved for a rare, ultra-severe form of inherited high cholesterol. But it requires monthly infusions and has been costed at roughly US$400,000 a year in some pharmacoeconomic analyses.
CTX310 takes the same biology and pushes it into the “one-and-done” era. Instead of repeatedly neutralising ANGPTL3 protein, it alters the underlying gene in liver cells so that less protein is made at all.
This is not the first time in vivo CRISPR has worked in humans. Intellia’s NTLA-2001, for transthyretin amyloidosis, showed mean 87% reductions in circulating TTR protein at higher doses after a single infusion, again using an LNP-delivered CRISPR-Cas9 system directed at the liver.
The difference is scale of disease: transthyretin amyloidosis is a rare, often fatal disorder. High cholesterol and triglycerides sit behind a third of global deaths.
How does CTX310 compare with today’s cholesterol drugs?
On raw lipid numbers, CTX310 is not doing something we have never seen before. At its top dose, the roughly 50% fall in LDL and 55% fall in triglycerides sit in the same ballpark as what can be achieved by combining high-intensity statins with PCSK9 inhibitors in adherent patients.
The contrast lies in how that effect is delivered, and who pays for it.
1. Statins and ezetimibe: cheap but poorly adhered to
Generic statins such as atorvastatin and rosuvastatin can cost under US$10 for a month’s supply in the United States using discount cards—well under US$150 per year. Ezetimibe is similarly inexpensive.
Yet adherence is stubbornly poor. Retrospective analyses and registry data consistently show that 25–50% of patients stop statins within six to twelve months; long-term, as few as one in four may still be taking the drug as prescribed after several years. From a population-health perspective, this “adherence leakage” is a major reason why cholesterol remains poorly controlled even in wealthy health systems.
2. PCSK9 monoclonals and siRNA: potent but pricey
Injectable PCSK9 antibodies such as evolocumab (Repatha) and alirocumab can lower LDL by around 60% and have proven cardiovascular outcome benefits. But their economics are very different from generics. Repatha’s list price in 2025 is about US$573 per month, though Amgen now offers a direct-to-patient programme at US$239 a month—roughly US$2,900 per year.
Inclisiran (Leqvio), a twice-yearly siRNA injection targeting PCSK9, launched with a headline price in the US of roughly US$6,500 per year, though net prices vary and the NHS in England now pays far less under a population-health agreement.
These agents are powerful and, in many settings, cost-effective—but still require repeated injections and clinic infrastructure.
3. ANGPTL3 blockade today: a niche, ultra-high-cost product
Evkeeza, the ANGPTL3 antibody, is transformative for patients with homozygous familial hypercholesterolaemia. But with projected drug-only costs of around US$400,000 per person per year (before administration costs), it was never intended for the tens of millions with more common lipid disorders.
4. CTX310’s pitch: one bill, 20-plus years of benefit?
CRISPR Therapeutics’ chief executive has suggested that CTX310’s eventual price is “very likely” to be under US$100,000 for a single infusion—hardly cheap, but an order of magnitude below ex vivo CRISPR therapies such as Casgevy for sickle cell disease, which carries a US$2.2 million list price.
If, in a best-case future, one infusion given in middle age kept LDL and triglycerides suppressed for 20 years or more, the notional annualised drug cost might look closer to US$5,000. That would still be vastly more expensive than generic statins—but potentially competitive with PCSK9 inhibitors and siRNA drugs, particularly if the treatment prevented downstream heart attacks, strokes and procedures.
At this stage, however, those are thought experiments, not data. We do not yet know how long CTX310’s effect will last in humans, whether durability will be uniform across patients, or whether late safety issues will emerge that alter the risk–benefit calculus.
The uncomfortable word: irreversible
The most important difference between CTX310 and essentially every existing cholesterol drug is not its potency. It is irreversibility.
A statin can be stopped. A PCSK9 injection wears off in months. If a rare side effect emerges, the drug can be discontinued. Gene editing in the liver, by design, cannot be “un-edited”.
The precedent from other CRISPR programmes is cautiously encouraging. NTLA-2001’s early ATTR amyloidosis data showed deep and apparently durable knockdown of TTR protein with only mild adverse events at 28 days, and longer-term follow-up has so far been acceptable. Ex vivo therapies such as Casgevy have also looked clinically impressive in small numbers of patients, with many achieving freedom from pain crises.
But the wider gene-editing field has had reminders that delivery vehicles and off-target effects matter. Verve Therapeutics paused its first base-editing trial (VERVE-101) for LDL lowering after a participant experienced thrombocytopenia and liver-enzyme elevations, later pivoting to a reformulated candidate, VERVE-102. More recently, the FDA placed a clinical hold on Intellia’s late-stage ATTR programme after a participant developed severe liver injury, highlighting how even liver-specific LNP gene editing can trigger unexpected toxicity.
Regulators have responded by requiring very long follow-up: CTX310 trial participants will be monitored for at least a year, with the option of 15 years of additional observation—mirroring gene-therapy frameworks for other products.
For a rare, otherwise fatal condition, patients and clinicians may accept a higher degree of uncertainty. For a middle-aged adult whose main problem is a future probability of heart attack, the risk tolerance is different. The bar for safety—for the LNPs, the CRISPR machinery and off-target edits—will be correspondingly high.
Will gene editing compete with, or complement, existing care?
A temptation in coverage of CTX310 has been to cast it as a potential replacement for statins, PCSK9 inhibitors and lifestyle change. That is premature, and arguably the wrong frame.
There are at least three more nuanced use-cases where a “one-and-done” ANGPTL3 edit might make sense if larger trials confirm efficacy and safety:
- Genetic and extreme risk
Patients with homozygous or severe heterozygous familial hypercholesterolaemia, or with combined severe hypertriglyceridaemia and LDL elevation, remain poorly served despite maximal drugs. CRISPR Therapeutics is explicitly prioritising severe hypertriglyceridaemia and mixed dyslipidaemia in its next-stage cohorts. - Failure or intolerance of standard therapy
A subset of patients simply cannot tolerate statins or maintain long-term adherence to injectables, despite clear evidence of benefit. For them, a one-time edit could, in theory, provide risk reduction that is otherwise unreachable. - Early-life risk management
Mendelian randomisation studies suggest that lifelong exposure to lower LDL delivers far more protection against coronary disease than lowering LDL later in life—roughly threefold greater risk reduction per mmol/L drop compared with short-term drug trials. A carefully selected group of younger, high-risk individuals might therefore gain disproportionate benefit from an early edit—though this is where ethical and regulatory concerns become most acute.
In all scenarios, CTX310 looks more like a potential layer on top of lifestyle measures and cheap generics than a wholesale replacement. Even investigators involved in the trial have emphasised that the therapy is being tested as an add-on, not a stand-alone cure.
Economics: who pays for editing risk?
The experience with gene therapies for rare blood disorders offers a cautionary template. Casgevy and its lentiviral rival Lyfgenia come with US list prices of US$2.2 million and US$3.1 million respectively, prompting intense debate about affordability even though they may cure otherwise devastating diseases.
Health economists point out that cardiovascular risk reduction is an even bigger market but a harder one to price. Heart disease is common, competing therapies are cheap for many patients, and payers worry about spending large sums today for benefits that may not materialise for years—especially in systems where patients frequently change insurers.
Some of the likely questions for CTX310 and similar therapies:
- How certain is durability?
Payers will want evidence that LDL and triglycerides remain substantially lower for a decade or more, not just 12–24 months. - Will regulators demand cardiovascular outcome trials?
For chronic LDL-lowering drugs, large outcome trials showing reductions in heart attack, stroke and cardiovascular death have become standard. It is hard to imagine a one-shot gene edit being widely reimbursed without similar evidence. - Can pricing be tied to outcomes?
Ex vivo gene therapies have experimented with instalment payments and outcome-based contracts. A similar model—spreading cost over many years and clawing back payment if benefits fade—may be needed to make “once-and-done” editing politically and economically acceptable at scale. - What about equity?
Cardiovascular deaths are disproportionately concentrated in low- and middle-income countries. If gene editing for cholesterol becomes available only to well-insured patients in wealthy systems, we risk widening an already large gap in heart-disease outcomes.
These are not primarily scientific questions. They sit at the intersection of health-economics, regulation and political will.
A broader pivot in cardiovascular therapy
CTX310 is part of a wider shift in how cardiometabolic risk might be managed. A recent review of RNA- and gene-editing therapies for cardiovascular disease argues that 2025 marks the beginning of a pivot away from chronic daily pills towards a mix of long-acting injectables (antisense oligos and siRNAs) and permanent “one-and-done” edits for selected risk factors.
Other players are pushing in parallel:
- Verve Therapeutics is developing base-editing treatments that permanently inactivate PCSK9 in the liver, with interim data suggesting very large LDL reductions before safety concerns forced a reformulation and closer scrutiny of LNP toxicity.
- CRISPR Therapeutics’ own CTX320 programme targets LPA, encoding apolipoprotein(a), in a bid to lower lipoprotein(a), a genetically determined risk factor that is difficult to treat with conventional drugs.
- RNA-based drugs aimed at Lp(a) and other targets are moving through phase 2 and 3, showing >90% reductions with dosing intervals measured in months rather than days.
Taken together, these pipelines suggest a future in which cardiologists and primary-care physicians may be choosing between:
- Daily oral drugs (statins, and perhaps oral PCSK9 inhibitors now in late-stage testing).
- Twice-yearly or yearly injections (siRNAs and other RNA-targeted agents).
- Single-course genetic interventions (CRISPR or base editing) for carefully selected patients.
The clinical question is not whether gene editing is “better” in the abstract, but for whom, under what circumstances, and at what price compared with these alternatives.
What this tiny CTX310 trial does and does not tell us
From a scientific standpoint, the CTX310 data are undeniably important. They show that:
- In vivo CRISPR editing delivered by LNPs can reliably and deeply knock down a cardiovascular risk gene in humans.
- Doing so can cut both LDL cholesterol and triglycerides by about half, on top of existing therapies, in high-risk patients.
- At least in the short term, this can be done without obvious serious toxicity in a small cohort.
But they do not yet tell us:
- How long the lipid reductions will last—five years, ten, or a lifetime.
- Whether gene-edited patients will actually experience fewer heart attacks and strokes than those on optimised conventional therapy.
- How frequently rare but serious adverse events will occur once hundreds or thousands of patients are treated.
- How regulators and payers will translate biomarker data into coverage decisions.
For now, CTX310 should perhaps be seen less as a looming product and more as a proof-of-concept: that the same CRISPR technology used to treat rare blood and nerve diseases can be aimed at the far more prosaic, but vastly more common, problem of cholesterol and triglycerides.
If future phases bear out the promise—and that remains a big “if”—cardiovascular prevention could shift from nudging patients to take tablets every day to offering some of them a single edit that quietly rewrites their long-term risk.
That prospect is exciting. It is also exactly the kind of change that demands slow thinking: not just about molecular off-targets, but about price, access, equity and what it means to permanently alter biology for conditions that many people still treat with a pill and a reminder app.
This article is for information and analysis only and does not constitute medical advice. Patients should discuss treatment options and trial participation with their own clinicians.